Research Article - (2024) Volume 11, Issue 3
Received: Sep 23, 2024, Manuscript No. JEBMH-24-148650; Editor assigned: Sep 26, 2024, Pre QC No. JEBMH-24-148650 (PQ); Reviewed: Oct 11, 2024, QC No. JEBMH-24-148650; Revised: Oct 18, 2024, Manuscript No. JEBMH-24-148650 (R); Published: Oct 25, 2024, DOI: 10.18410/ jebmh/2024/11/04:1-6
Citation: Shafna K T, Lubaiba VP, Vineetha P. Ultrasound Guided Airway Parameters for Predicting Difficult Airway in Adults. J Evid Based MedHealth 2024;11(04):1-6.
Aim
Ultrasonography is a non-invasive bedside device for predicting difficult airways. This study aims to evaluate whether ultra-sonographic airway parameters such as the ratio of Pre-Epiglottis space (Pre-E) depth to the distance measured from epiglottis to midpoint of distance present between the Epiglottis Vocal Cords (E-VC), a ratio of Hyomental Distance(maximal/neutral) (HMDR(m/n)) and Tongue Thickness (TT) could be used in predicting Difficult Airway (DA).
Materials and Methods
After getting research and ethical committee approval, Pre-E/E-VC ratio had been measured using a linear USG probe and HMDR(maximal/neutral) ratio and TT were measured using a curved probe preoperatively on the day of surgery. Cormack Lehane grading was noted during direct laryngoscopy after general anesthesia induction. The predictive value of each parameter was measured by employing Negative Predictive Value (NPV), sensitivity, Positive Predictive Value (PPV), as well as specificity. ROC analysis had been done to identify each parameter’s cut-off value to predict difficult airway.
Results
Out of the three airway parameters studied in 210 patients, Pre-E/E-VC ROC analysis revealed a threshold of >0.73, sensitivity 80%, specificity 85.1%, PPV 51.8% and NPV 95.5%. HMDR(maximal/neutral) showed a sensitivity of 97.1%, specificity 72% and a cut-off of ≤ 1.21. Tongue thickness with a cut-off of ≥ 5.2cm showed lowest sensitivity 60% and specificity 55.4%.
Conclusion
This study concluded that ultra-sonographic airway parameters are useful in predicting difficult airway preoperatively. HMDR(m/n) has a maximum sensitivity of 97.1% and specificity of 72%, while Pre-E/E-VC has a maximum specificity of 85.1% and sensitivity of 80%. A threshold of HMDR(m/n) ≤ 1.2 as well as Pre-E/E- VC of ≥ 0.73 could be utilized should anticipate a DA.
Anesthesia, General, Intubation, Laryngoscopy, Ultrasonography.
Airway management is one of the main challenges to an anesthetist. Higher inter- observer variability along with the use of airway assessment screening measures with low predictability may be the cause of the inability to predict a difficult airway prior to surgery [1,2]. A safe and non-invasive method of diagnosing and precisely imaging airway structures for quick airway assessment is called airway sonography [3-5]. In emergencies and unconscious patients, ultrasound examination of the upper airway is a useful technique for anticipating a difficult airway, particularly in cases when palpating anatomic features is challenging [6,7].
It can be used to assess the size of the endotracheal tube, confirm the correct placement of the tracheal tube and laryngeal mask, diagnose pathology of the upper airway and guide percutaneous tracheostomy and cricothy roidotomy [8]. Preoperative airway assessment can be done clinically using Modified Mallampati classification, thyromental distance, neck movements, upper lip bite test, mouth opening, etc. The Cormack-Lehane (CL) grade of laryngeal view is used to describe the appearance of the laryngeal inlet during direct laryngoscopy [9]. However, these tests alone do not predict difficult airways where the Cormack Lehane (CL) 3 and 4 grades represent difficulty and 1 and 2 represent easy intubation [10]. Now, USG is a part of an anesthetist’s tool kit to help with various procedures ranging from elective care to emergencies.
Sound waves which produce images of structures through which they travel are used in USG [11]. Because of its wide field view, the low-frequency curved probe is utilized to provide sagittal and parasagittal images of submandibular and supraglottic structures, while the high-frequency linear probe is used to image superficial airway structures [12].
Various ultrasound-guided parameters have been used for preoperative airway assessment. Measurements including tongue thickness, volume, cross-sectional area, hyoid and vocal cord thickness, pre-epiglottis gap thickness, Hyomental Distance Ratio (HMDR) and soft tissue thickness of the anterior neck were previously evaluated to predict challenging airway situations [13,14]. The current study goal is to determine the predictive value of ultra-sonographic measurements such as Tongue Thickness (TT), Hyomental Distance Ratio(maximal/neutral) positions (HMDR(m/n)) and ratio of pre-epiglottic space depth to distance from epiglottis to vocal cords midpoint (Pre E/E-VC) for difficult airway and to determine the cut-off value of each parameter to predict the same.
This observational study was done in the main operation theatre complex of a tertiary care teaching hospital during the period from June, 2021 to July, 2022. The formula used for sample size calculation is,
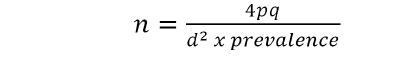
Substituting the values of p and q from the parent study by S Rana et al., where p is the sensitivity of Pre E/E-VC to predict difficult laryngoscopy, which is 82% and q=100–p which is 18%. Precision (d) was taken as 15% and prevalence which was the proportion of difficult intubation, was taken as 0.125. Substituting the values to the above equation, the sample size calculated was 210.
Inclusion Criteria
The study included 210 patients between the ages of 18 and 65 who were undergoing general anesthesia with endotracheal intubation for surgery and had an American Society of Anesthesiologists Physical Status (ASA PS) of 1 or 2.
Exclusion Criteria
Patients who needed rapid sequence intubation, non- cooperative patients, those having limited cervical spine mobility and maxillofacial anomalies, ASA PS III and IV and antenatal patients were excluded from the present study subjects were selected by convenient sampling technique and all 210 patients completed the study and no one was excluded.
During routine preoperative visits, written informed consent was taken and an airway assessment was done using Mallampati Classification (MMC). Easy airway was anticipated for Mallampati class 1or 2 and difficult airway for class 3 or 4. the USG machine were used to measure the sonographic parameters. Utilizing a high-frequency linear probe, the pre- epiglottis space was located, keeping the probe in the midline submandibular area. The epiglottis and posterior portion of vocal cords with arytenoids can be seen together on the screen by rotating the probe from the cephalad to the caudal direction in the transverse plane. Vocal cords were visualized as hypoechoic structures in triangular shape with vocal ligaments as hyperechoic structures at their medial border. The epiglottis has been seen as a hypoechoic structure with a curvilinear shape. The same probe was used to measure the Pre- Epiglottis space (Pre-E) depth and the distance between the Vocal Cords’ mid-points (E-VC) and the epiglottis and the ratio was computed. In a similar way, visualization of the tongue and the shadows cast by the mandible and hyoid bone was facilitated by a curved lower-frequency probe which have been placed in the submental region in the midsagittal position. The Hyomental Distance (HMD) has been calculated between the posterior aspect of symphysis mentis and the anterior margin of the hyoid bone. The Hyomental Distance ratio (maximal/neutral) was calculated by dividing the HMD measurement with the head in full extension to that in the neutral position respectively. The USG probe was held sub mentally in the median sagittal plane to calculate the maximal vertical distance between the tongue surface & the submental skin in order to assess Tongue Thickness (TT).
The attending anesthetist’s discretion, the patients who were moved to the operating room received conventional general anesthetic care. Following induction, a senior anesthetist with over five years of experience, who was blinded for the USG measured parameter, performed direct laryngoscopy using a properly sized curved Macintosh blade. According to Cormack Lehane (CL) grading, grades 1 and 2 classified as easy, whereas grades 3 and 4 as difficult. Intubation was done with an appropriate-size endotracheal tube and anesthesia was maintained. Only the best attempt at direct laryngoscopy, achieved by optimal posture and total muscle relaxation, was recorded. A proforma that was structured was used to gather data.
Statistical Analysis
R software was used for analysis and Microsoft Excel 365 software was used for data entry. The continuous variables like age and USG parameters were summarized as mean and standard deviation. Age was also categorized into intervals of 10. Categorical variables like gender, ASA class, MMC Class and Cormack-Lehane class were summarized as frequency and proportions. An unpaired t-test was done for comparing the different USG parameters of the neck between the patients with difficult intubation and easy intubation. ROC analysis was done to find out the cut-off value for each parameter to predict a difficult airway. To evaluate the predictive value of each parameter, the following metrics were computed: specificity, sensitivity, Positive Predictive Value (PPV) and Negative Predictive Value (NPV).
210 patients meeting inclusion criteria were enrolled in present study. The maximum number of patients (65 patients) were 20 years-29 years (30.95%) of age (mean ± SD 36.6 ± 11.9) (Figure 1).
There are 210 patients, among them 48.1% were males and 51.9% were females (Figure 2). The patients belonged to ASA PS 1 grading was 63.8% and the rest 36.2% were ASA PS II (Figure 3). Based on the conventional airway assessment, 104 (49.5%) belonged to the MMPC 1 category, 75 (35.7%) to MMPC 2 and 31 (14.8%) to MMPC 3. No patients were reported to have MMPC 4 (Figure 4).
The ratio of the pre-epiglottis space depth to the distance from the epiglottis to the middle of vocal cords’ distance (Pre E/E- VC), the Tongue Thickness (TT) and the Hyo Mental Distance Ratio (HMDR(m/n) ) were the airway parameters measured by USG in this research. Out of 210 participants; 92 (43.8%) belonged to CL I grade, followed by 83 (39.5%) in CL II, 31 (14.8%) in CL III and 4 (1.9%) in CL IV. The CL grade distribution predicted from USG measured Pre-E/E-VC ratio were 0.57 ± 0.14; 0.59 ± 0.17 (mean ± SD) for grades 1,2 and 1.08 ± 0.48; 1.36 ± 0.48 for grades 3,4 (p=0.0001) respectively (Tables 1 and 2). An AUC of 0.84 (95% CI 0.74- 0.94) was found using ROC analysis and a cut-off of Pre-E/ E-VC ≥ 0.73 was shown to predict difficult intubation with a specificity and sensitivity of 85.1% and 80%, correspondingly. The Pre-E/E-VC ratio has a PPV of 51.8% and a NPV of 95.5% (Table 3 and Figure 5). Whereas, the CL grade distribution with HMDR(maximal/neutral) were 1.26 ± 0.10; 1.30 ± 0.14 (mean ± SD) for CL 1,2 respectively and 1.06 ± 0.08; 1.04 ± 0.01 for CL 3 and 4 (p=0.0001) (Table 1). We could find that as the HMDR(maximal/neutral) value decreases, the CL grade increases leading to difficult intubation. With a cut-off of HMDR(m/n) ≤ 1.21, ROC analysis depicted an AUC of 0.95 (95% CI 0.90-1.0), indicating difficult intubation with a specificity and sensitivity of 72% and 97.1%, correspondingly. The positive Predictive Value for HMDR(maximal/neutral) is 44.6% and the Negative Predictive Value 98.5% (Table 3 and Figure 6). While analyzing Tongue Thickness (TT), we found that as TT increases, CL grade also increases. Distribution of this parameter with CL grade showed 4.97 ± 0.53; 5.06 ± 0.52 (mean ± SD) for CL grade 1 and 2, 5.35 ± 0.58; 5.54 ± 0.70 for CL grade 3 and 4 respectively (Table 1). ROC analysis of TT depicted an AUC of 0.67 (95% CI 0.56–0.78), with a cut-off of TT ≥ 5.2cm predicting difficult intubation with a sensitivity of 60% and specificity of 55.4%. The PPV is very low for tongue thickness 22.1% while the NPV is 87.4% (Table 3 and Figure 7). We compared all three USG parameters of the neck between patients with difficult and easy intubation and found statistically significant for predicting difficult intubation (p<0.001). Similarly, we got a significant association for MMC with CL and all the above USG measured parameters in predicting difficult airways (p<0.05) (Tables 4 and 5). So we could conclude that all three USG measured airway parameters are effective in predicting difficult laryngoscopy. HMDR(m/n) has had a maximum sensitivity of 97.1% while Pre- E/E-VC has had a maximum specificity of 85.1% and sensitivity of 80%. A cut-off value of HMDR(m/n) ≤ 1.21 and a Pre-E/E-VC ratio ≥ 0.73 can be utilized to predict difficult laryngoscopy preoperatively.
| Parameter | CL 1 (n=92) | CL II (n=83) | CL III (n=31) | CL IV (n=4) |
|---|---|---|---|---|
| Pre E/E-VC* | 0.57 (0.14) | 0.59 (0.17) | 1.08 (0.48) | 1.36 (0.48) |
| HMDR m/n* | 1.26 (0.10) | 1.30 (0.14) | 1.06 (0.08) | 1.04 (0.01) |
| TT* | 4.97 (0.53) | 5.06 (0.52) | 5.35 (0.58) | 5.54 (0.70) |
| Parameter | CL 1 & 2 | CL III & IV | p-value* |
|---|---|---|---|
| Easy intubation | Difficult intubation | ||
| (n=175) | (n=35) | ||
| Mean (SD) | Mean (SD) | ||
| Pre E/E-VC | 0.58 (0.15) | 1.11 (0.48) | <0.001 |
| HMDR m/n | 1.28 (0.12) | 1.06 (0.07) | <0.001 |
| TT | 5.02 (0.53) | 5.37 (0.58) | <0.001 |
| Para meter |
Sensitivity% | Specificity% | PPV% | NPV% |
|---|---|---|---|---|
| Pre E/E-VC | 80.0 | 85.1 | 51.8 | 95.5 |
| HMDR m/n | 97.1 | 72.0 | 44.6 | 98.5 |
| TT | 60.0 | 55.4 | 22.1 | 87.4 |
| MMC | Total predicted(N) | Difficulty based on CL | p-value* | |
|---|---|---|---|---|
| Easy (N) | Difficult (N) | |||
| Easy (N) | 179 | 169 | 10 | p<0.05 |
| Difficult (N) | 31 | 8 | 23 | |
| Total | 210 | 177 | 33 | |
| MMC | Difficulty based on | p-value* | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre E/E-VC | HMDR (m/n) |
TT | Pre E/E-VC | HMDR (m/n) | TT | |||||
| E | D | E | D | E | D | 0.000 |
0.000 |
0.000 | ||
| E | 179 | 154 | 25 | 119 | 60 | 100 | 79 | |||
| D | 31 | 2 | 29 | 1 | 30 | 11 | 20 | |||
| 210 | 210 | 210 | 210 | |||||||
Airway management remains biggest challenge to the anesthesiologist and maintaining a patent airway is of utmost concern. Although the Mallampati class is the most frequently utilized clinical parameter for predicting the difficult laryngoscopy, the accuracy of difficult airway prediction may be affected due to subjective variation. Even after the most careful preoperative airway evaluations, some patients with a difficult airway remain undetected. Ultrasound is now rapidly developing in the field of anesthesia ranging from its use in various regional blocks and central venous catheter insertion to its use in anticipation of difficult airways. Airway imaging is a newer application of Ultrasound that has been widely used for diagnosing upper airway pathology [15,16]. It has become an effective tool for the anesthetist in acute and elective care of a patient’s airway and thus its use in difficult airway management is fundamental [17-19]. A combination of ultra-sonographic and clinically measured parameters leads to better prediction of difficult laryngoscopy and intubation. Favorable results have been obtained from a few studies that utilized ultra-sonographic measured airway parameters to predict difficult laryngoscopy of the 210 patients that participated in this trial, 35 had a difficult airway, classified as CL grade 3 or 4. With a mean age of 36.6 ± 11.9 years, the majority of patients (30.95%) belonged to the 20 years–29 years age group and 63.8% were classified as ASA I. All the three airway parameters studied by USG preoperatively, Pre-E/E-VC, HMDR(maximal/neutral) and TT were shown to have a significant association in predicting difficult airway (p<0.05). The sensitivity and specificity for Pre E/E-VC ratio were 80% and 85.1% respectively and 97.1% and 72% for HMDR(m/n) making these parameters good for predicting difficult airway. The cut-off score for predicting difficult laryngoscopy was ≥ 0.73, ≤ 1.2 and ≥ 5.2cm for Pre-E/E-VC, HMDR(maximal/neutral) and TT respectively. S Rana et al., conducted a study on 120 patients that showed a 12.5% incidence of difficult intubation. Both Pre-E/E-VC and HMDR depicted a highly significant association with CL grading in predicting difficult airways (p<0.05). Pre-E/E-VC showed a sensitivity of 82.1%, specificity of 80%, NPV of 92.3% and PPV of 60.5% while for HMDR, the values are 75%, 85.3%, 90.1% and 65.6% respectively [20]. In the current study, the sensitivity and specificity of Pre-E/E-VC were similar to the above study (80% and 85.1% respectively) and became a good predictor of difficult airway. Similarly, this study also showed that HMDR(maximal/neutral) for predicting difficult airways had 97.1% sensitivity and 72.1% specificity. The cut-off score derived by S Rana et al., for Pre-E/E-VC and HMDR(maximal/neutral) was 1.77 and 1.0850 while we got the values 0.73 and 1.21 respectively.
P B Reddy et al., showed a 14% incidence of difficult intubation in 100 patients. They concluded that the Pre-E/E-VC ratio had a low to moderate predictive value with a specificity of 86.7% [8]. In the present study, we got 80% sensitivity and 85.1% specificity for Pre-E/E-VC ratio with a cut-off score of ≥ 0.73 which makes this parameter a better predictor of the difficult airway.
J Huh et al., evaluated the HMDR ratio in 213 patients and it had the highest sensitivity (88%) with a relatively low specificity (60%) and a PPV of 23% [21]. In the present study, we find that as HMDR(maximal/neutral) decreases, CL grade increases and predicts a difficult airway with 97.1% sensitivity and 72.0% specificity. Wojtczak et al., concluded that the ultrasound- guided HMDR was a good predictor of the difficult airway while the current research also showed that HMDR is effective in predicting difficult airway with 97.1% sensitivity and 72% specificity with a cut-off value ≤1.21 [22].
A study by Yao et al., concluded that increased tongue thickness was an independent predictor for difficult airway and intubation with 75% sensitivity, 72% specificity and an AUC of 0.78 [23]. The present study reveals the cut-off value for TT as ≥ 5.2cm with 60% sensitivity, 55.4% specificity, 22.1% PPV and 87.4% NPV. A study by Sanyal et al., found that the Mallampati class had low sensitivity and positive predictive value (42.86% and 28% respectively) for predicting difficult airways whereas the specificity was 82.56%. He thus concluded that for preoperative airway assessment, the Mallampati test should be supplemented by other airway assessment tools [24]. Whereas according to the research by Kalezic et al., the sensitivity and specificity of the Mallampati score were 64% and 61.5% respectively and thus concluded that the Mallampati score is a significant predictor of difficult laryngoscopy [25].
As per the current study also, MMC showed a significant association with CL grading and USG-measured airway parameters for predicting difficult airway (p<0.05). Hence along with the clinical measures, the inclusion of the ultrasound- guided airway parameters may help to improve the difficult airway prediction.
This study found that the following ultrasonography-measured airway parameters are significant predictors of difficult airway: Tongue Thickness (TT), depth of pre-epiglottis space to distance from epiglottis to midpoint of the distance between vocal cords (Pre-E/E-VC) and HMDR(m/n). When it comes to predicting difficult airways, HMDR has a higher sensitivity of 97.1% and a specificity of 72%, whereas Pre-E/E-VC has an 80% sensitivity and an 85.1% specificity. Tongue thickness showed low sensitivity and specificity 60% and 55.4% respectively compared to the other two parameters.
Institutional Research and Ethical Committee (IEC) approval was obtained with the corresponding IEC number: GMCKKD/ RP2021/IEC/137.
The major limitations included the observational nature of the study and increased chances of inter-observer variations during laryngoscopic assessment and Cormack Lehane grading. And we did not include patient groups having a high chance of difficult intubation such as pregnancy, obesity, etc. Since external laryngeal manipulation usually facilitates intubation, difficult laryngoscopy does not always leads to difficult intubation.
[Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]